Introduction
Physical therapy in Brooklyn for Stroke Rehabilitation
Welcome to Ari Levine PT, PC’s patient guide to Stroke Rehabilitation.
This guide will help you understand:
- how a stroke occurs and the difference between types of strokes
- how a stroke affects the body
- what rehabilitation after a stroke consists of
Anatomy
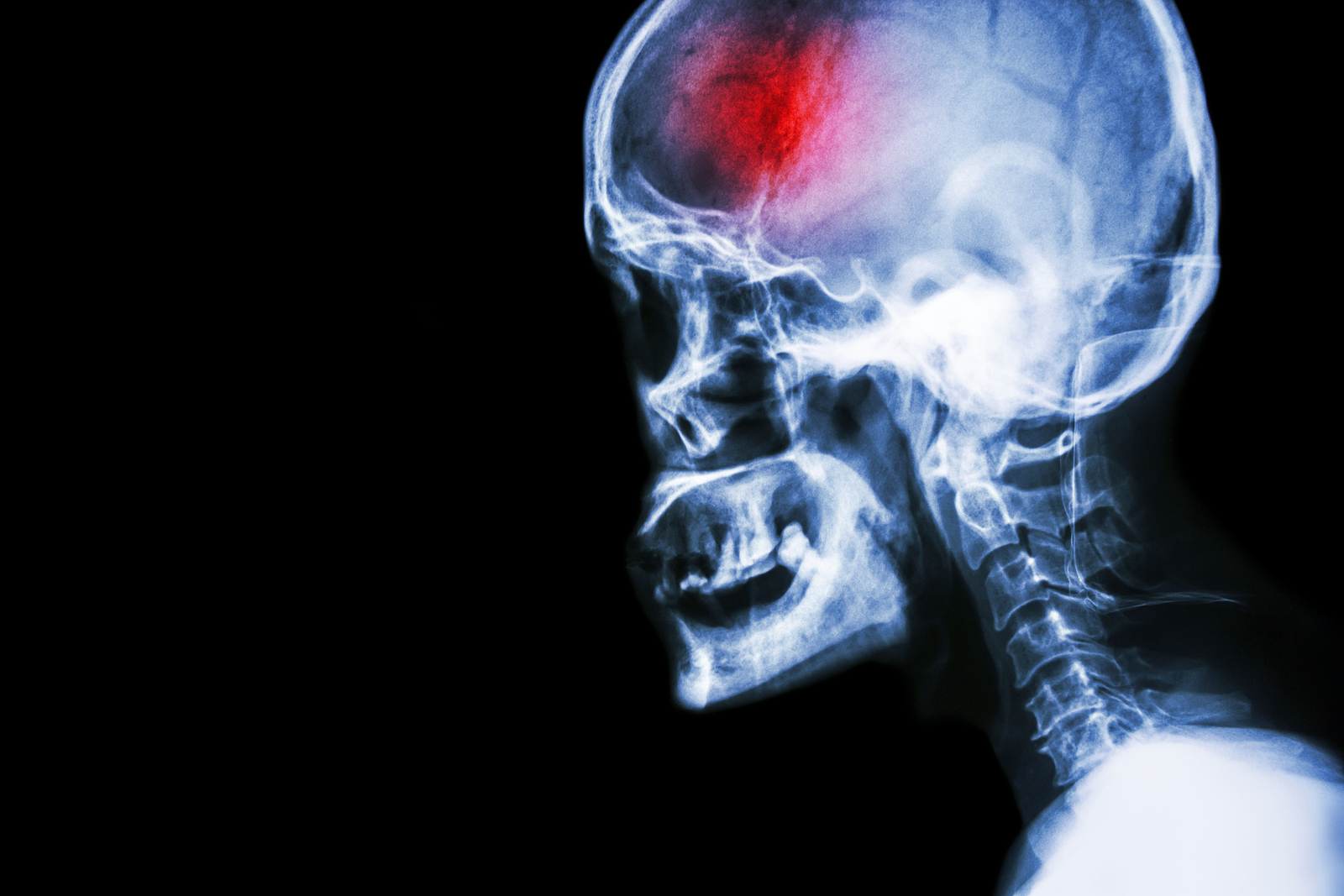
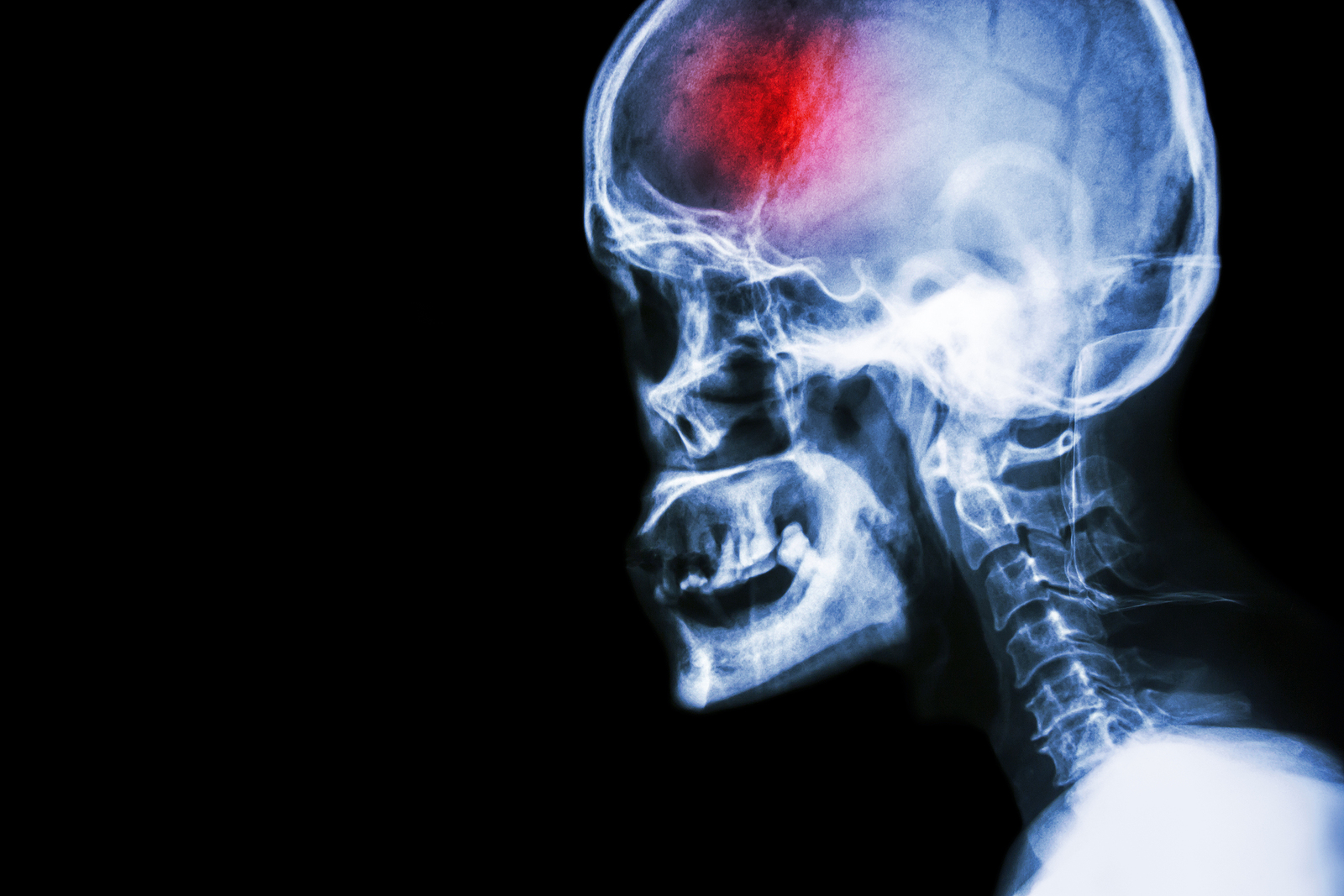
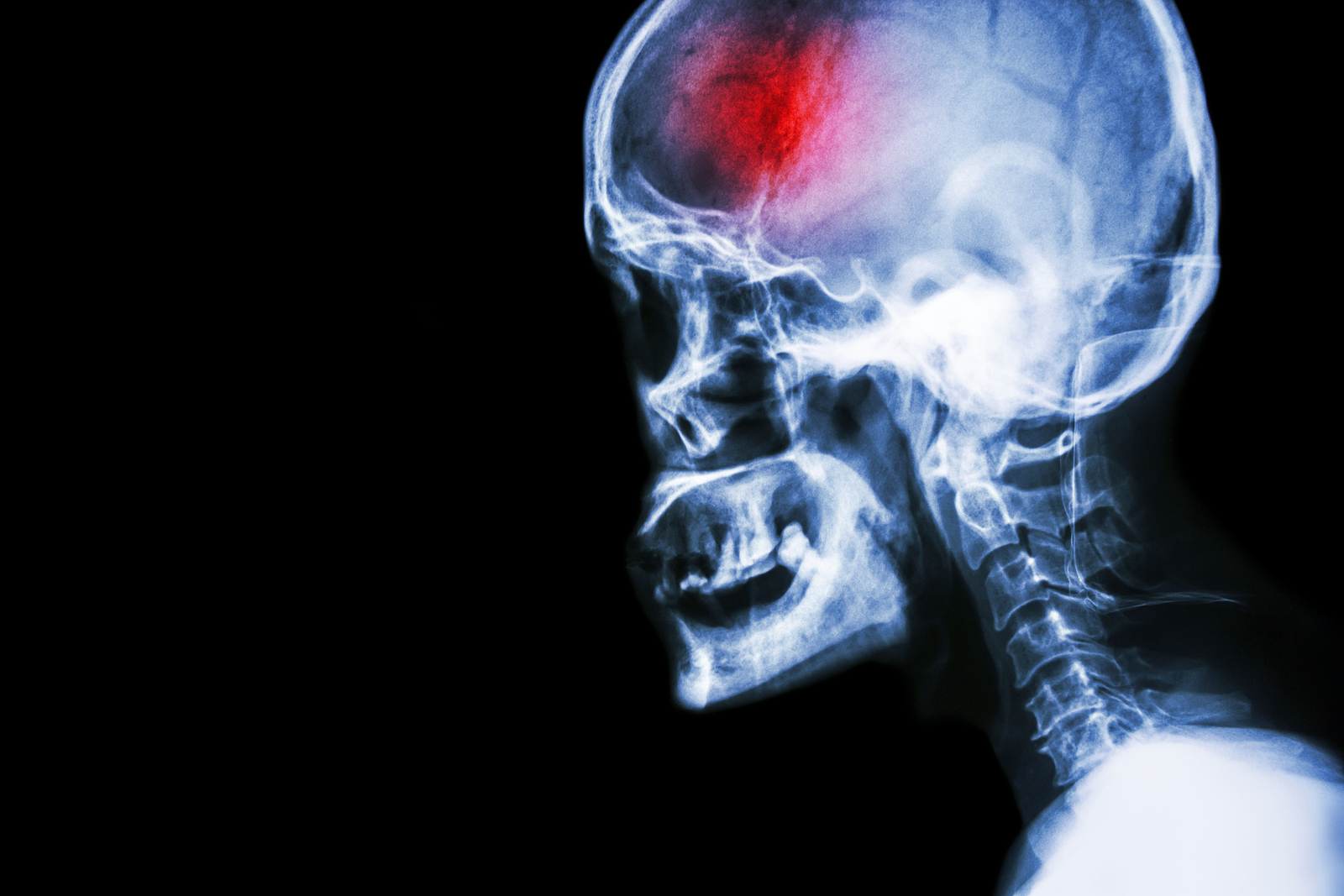
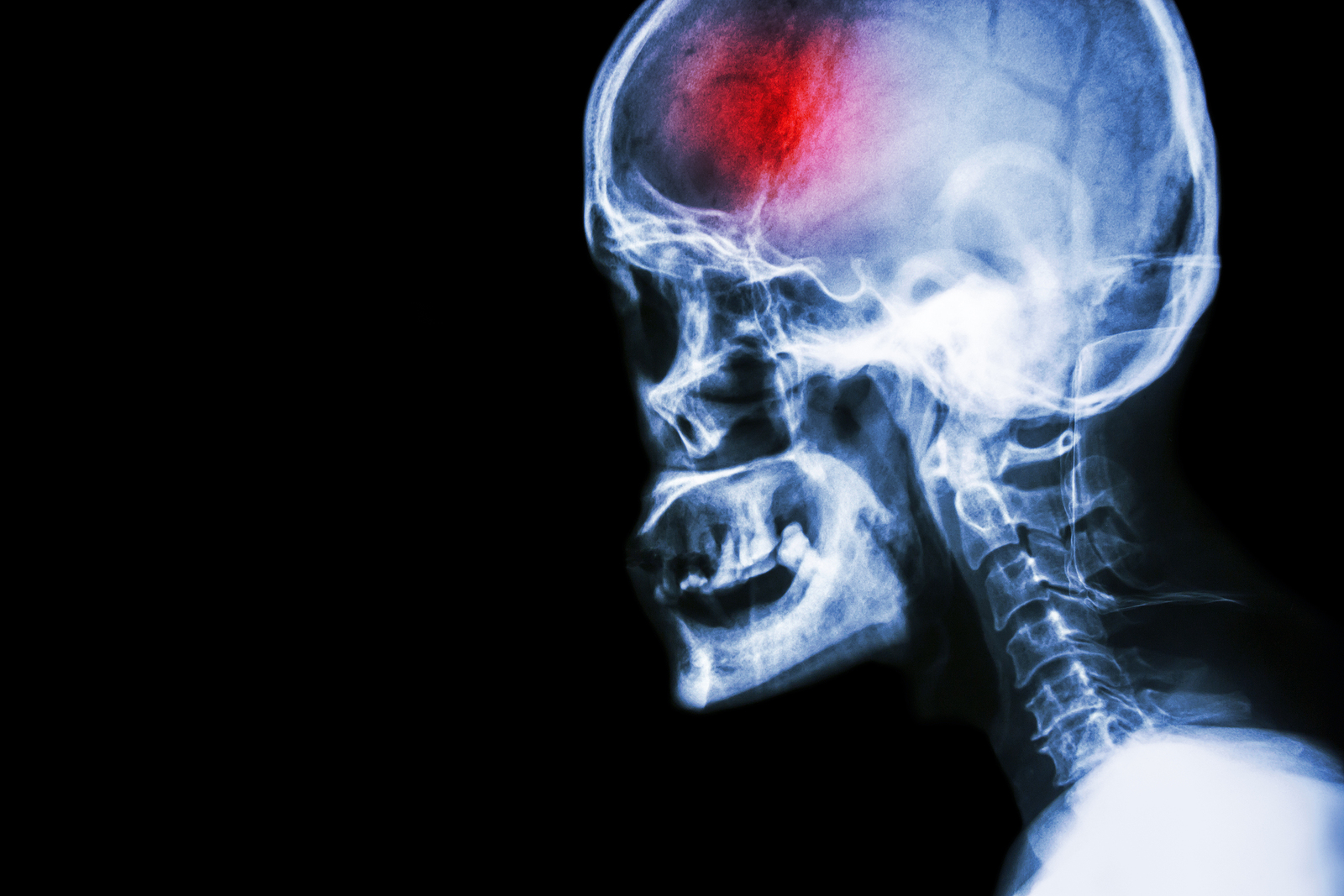
What is a stroke?
A stroke (previously known as a cerebrovascular accident) when there is a decreased flow of blood to the brain from either a blockage in the blood vessels that supply the brain (ischemic stroke), or a bleed from the blood vessels that supply the brain (hemorrhagic stroke). When the blood flow to the brain is blocked it prevents the brain from getting the needed oxygen and nutrients to function. Without oxygen the brain cells can be permanently damaged or die and the physical and mental functions related to that area of the brain will be affected. A stroke is a medical emergency and rapid treatment is crucial to decreasing the damage caused by a stroke.
Signs and symptoms
Because a stroke disrupts the blood supply to the brain, many functions of the brain are immediately affected and are considered classic signs of a stroke in progress. These include:
- sudden slurred or incoherent speech
- sudden numbness or tingling in the face, arm or leg, or one side of the body
- inability to raise one arm in comparison to the other arm
- inability to smile on one side
- sudden slouching to one side in sitting
- drooping eye or mouth on one side
- sudden loss of mental capacity
- sudden severe headache
- sudden blurred or disturbed vision of one or both eyes
- sudden decrease or loss of consciousness
- sudden balance problems in sitting or walking
Types of strokes
There are three types of strokes:
- Ischemic stroke: a stroke that is caused by a blockage (clot) that disturbs the blood flow to the brain.
- Hemorrhagic stroke: a stroke that is caused by a bleed that disturbs the blood flow to the brain and puts pressure on the surrounding tissue.
- Transient ischemic attack: often referred to as a “mini-stroke” or TIA, where the blood flow to the brain is temporarily disturbed and as a result causes temporary signs and symptoms of a stroke that resolve quickly .
What happens with a stroke?
When any type of stroke occurs and the blood flow to the brain is compromised, all the functions which that part of the brain controls are subsequently disturbed. The brain on one side of the head controls the movement functions and sensation on the opposite side of the body. This means that if you have a stroke on the left side of the brain, the right side of the body will be affected. If the stroke is on the right side of the brain, the left side of the body will be affected.
Every stroke is unique depending on exactly which area of the brain has been affected. The bigger the bleed or blockage and the longer that the stroke goes without treatment (to stop the bleed or unblock the blockage), the more severe the impairments and the greater number of abilities that will be affected. It is worth reiterating that time is of the essence when a stroke first occurs; early treatment can immensely improve outcomes.
Ischemic Strokes:
Blood usually flows freely in our arteries to supply all areas of our body including our brain. Plaque, which is a fat-type substance coming from the food we eat, can build up along the walls of the arteries and cause them to harden (commonly referred to as hardening of the arteries), which leads to a condition called atherosclerosis. Atherosclerosis causes the arteries to lose their elasticity and become narrow. This limits blood flow in the arteries and increases one’s blood pressure. Although atherosclerosis can occur anywhere in the body, when it occurs in the arteries that supply the brain, including the carotid arteries in the neck, it is particularly risky for the plaques to break free and travel to the brain causing an ischemic stroke.
Hemorrhagic Strokes:
A bleed in the brain can occur due to several reasons. Aneurysms are balloon-like bulges in the brain that can burst causing a bleed. Aneurysms can be a malformation you are born with or can occur due to atherosclerosis.
Arteriovenous malformations (AVMs) are malformations that someone is born with which cause poorly formed arteries and veins within the brain. Having an AVM increases the chances of these vessels breaking open and causing a stroke. Bleeding in the brain disrupts the blood supply to the brain tissue along its path as well as causes pressure from the escaped blood to any surrounding tissue.
Transient Ischemic Attacks (TIAs):
TIAs are often called ‘mini-strokes’ and are warning signs that a larger stroke may be impending. TIAs do not cause lasting effects; numbness in the face or one side of the body, or vision or mental lapses may come and go, hence the name transient. Symptoms of TIAs should be heeded and promptly brought to the attention of a medical professional for early risk evaluation.
Risk Factors
There are several risk factors that make one more susceptible to having a stroke. These are:
- High blood pressure
- High levels of ‘bad’ cholesterol
- Diabetes
- Smoking
- Heart and blood vessel diseases
- Other medical conditions such as having sleep apnea, kidney disease, or bleeding disorders
- Certain medications (such as blood-thinners)
- Brain aneurysms or arteriovenous malformations (AVMs)
- Infections or conditions that cause inflammation, such as lupus or rheumatoid arthritis
- Age; as you age, your likelihood of having a stroke increases
- Sex; overall men are more likely to have a stroke but women’s likelihood increases as well as they age particularly past the age of 75
- Race and ethnicity; in North America higher rates of stroke are reported to occur among African-Americans, Hispanics and native Americans, however this may be a factor of racialized research with bias due to socioeconomics and access to health care, rather than a genetic predisposition.
- Family history of strokes
- Stress and anxiety, which can increase blood pressure
- Living in an area with higher air pollution
- Being overweight, particularly with extra weight around the abdomen
What does a stroke feel like?
If someone is educated on what the signs and symptoms of a stroke are then they may be aware of what is happening to them as the stroke occurs. Symptoms most often occur very rapidly but they can occur over several days (such as in TIAs) before an actual full stroke ensues.
During a stroke, someone may experience any of the symptoms listed above. Given that a stroke impairs brain function and subsequently the function of the body, someone may be aware of what is happening but will be unable to help themselves activate emergency medical help except perhaps in the cases of mild strokes or with a TIA. If a stroke is suspected, emergency medical assistance should be immediately activated as stroke recovery is highly dependent on how quickly treatment is triggered.
Diagnosis
The classic signs and symptoms of a stroke often create an obvious suspicion of stroke, however once at a medical centre, other objective tests are completed to confirm the stroke diagnosis. It is important for the medical team to determine which kind of stroke is occurring in order to assist with the most effective type of treatment.
Physical Examination: A physical exam to assess the function of your limbs, face, and mental capacity will be completed. In addition, your heart rate and blood pressure will be taken.
Blood Tests
Blood tests are completed to look for markers in your blood such as cholesterol, signs of infection, blood sugars, and the ability for your blood to clot.
Computed Tomography (CT) scan and/or Magnetic Resonance Imaging (MRI) scan: These tests are done on your brain and used to locate the exact location of the stroke and to determine if it has been caused by a blockage or a bleed. These tests can also help rule out other conditions that may be causing symptoms, such as an infection or a brain tumour
 Other tests
Other tests
Several other tests may be conducted to assist in diagnosing a stroke, such as echocardiograms to look at the heart, or ultrasounds to check for the state of the carotid arteries in your neck.
The effects of each stroke are unique depending on where the blockage or bleed occurs within the brain. The brain anatomy is similar in all individuals, so if a stroke occurs in the left side of the brain, the function of the right side of the body will be affected. If a stroke occurs in the right side of the brain, the left side of the body will be affected. If one side of the body is fully paralyzed, it is called hemiplegia. If one side of the body is only partially affected and shows weakness rather than paralysis, it is called hemiparesis.
The affected side of the body may initially experience what is called ‘neglect’ where the individual has difficulty even acknowledging that the affected side exists; the individual may struggle to turn their head to that side or even reach across and acknowledge the presence of that side of the body. This occurs more frequently and with greater severity when the right side of the brain has had the stroke and is termed “left-side neglect”. It can also occur when the left side of the brain has had the stroke and is then termed “right-side neglect”. This neglect often improves with rehabilitation.
Each half or hemisphere of the brain has particular responsibilities, so depending on which side the stroke occurs, there may be more impairment to certain brain functions. For example, a particular phenomenon can occur regarding language and communication. If the area of the brain known as Broca’s area is affected, a person who has suffered a stroke may be present with expressive aphasia where they know what they want to say, but have trouble saying or writing what they mean. Conversely, if Wernicke’s area is damaged, they may have receptive aphasia where they hear the voice or see the print, but can't make sense of the words.
The left side of the brain is more responsible for:
- Speech and language
- Chewing and swallowing
- Logic
- Mathematics
- Critical thinking
- Judgement/reasoning
The right side of the brain is more responsible for:
- Imagination
- Art
- Non-verbal cues
- Rhythm
- Intuition
- Attention span
- Visuospatial
Treatment
In order to most effectively treat your stroke, the medical team needs to determine whether the stroke is being caused by a blockage or a bleed as the treatments are very different.
Treatment for an ischemic stroke (blockage or clot)
In order to stop the damage being caused by a blocked artery in the brain, the clot needs to be dissolved or removed so blood flow to the brain can be restored. An intravenous injection into your arm with a drug called tissue plasminogen activator (tPA), which is also called Activase, is the most effective treatment for an ischemic stroke. This drug dissolves the clot which has caused the stroke and allows blood flow to the brain to be restored. In order to be effective tPA needs to be given within 4.5 hours of the onset of symptoms, hence the urgency in diagnosing the type of stroke and the necessity to receive prompt medical attention when a stroke is suspected.
In some cases of an ischemic stroke it is determined that the clot needs to be directly treated. In these cases the medical team may decide to do a more invasive procedure where they go right into the blood vessels to get at the clot (endovascular procedure). Doctors can insert a tube (catheter) through the blood vessels in the groin that then follows the blood vessels up to the brain. tPA may be directly administered to the area of the clot, or the clot may be able to be removed with a device attached to the catheter.
Treatment for a hemorrhagic stroke (brain bleed)
In order to stop the damage being caused by a bleed in the brain, the bleed needs to be stopped so that the normal blood flow to the brain can be restored and the pressure from the extra blood in the brain can be reduced. If you are on blood thinning medication then these medications will be stopped immediately. Surgery may be performed to clamp the bleed or aneurysm or to remove an atrial-venous malformation (AVM). Clotting may be encouraged at the site of the bleed with small coils inserted through a catheter in the groin which leads up to the area of the bleed in the brain.
Treatment for transient ischemic attacks (TIAs)
In order to decrease the chance of having a full-blown stroke, doctors may choose to ‘clean out’ the blood vessels in the neck that lead up to the brain (carotid arteries). In this procedure, called a carotid endarterectomy, the plaque that has built up in these arteries is cleared out. This may also be done after a patient has already had a stroke, if the clogged carotid arteries have been determined to be the source of the original clot.
Another technique to unblock the carotid arteries and decrease your chance of having a stroke is for doctors to perform an angioplasty, in which a small catheter with a mini deflated balloon is inserted into an artery in your groin and threaded up to the arteries in your neck. The balloon is then re-inflated to push the clogging plaque out of the interior of the arteries and open the vessel, which creates more room for the blood to flow. A stent, which is a solid structure that helps to maintain the open artery, can then be placed inside to keep the artery patent. Your doctor may also choose to start you on blood thinning medication to reduce the chance of a clot forming.
Reducing the likelihood of plaque build up in your arteries can significantly reduce your risk of having a stroke. Leading a healthy lifestyle including a mindful diet low in processed foods and fats, participating in regular exercise, modifying your stress and avoiding or quitting smoking can significantly reduce your risk of having a stroke.
Rehabilitation
Every stroke that occurs is unique. Each is dependent on where in the brain the bleed or blockage occurs as well as how long it took for treatment to be administered. As mentioned before, there will most often be one side that is physically affected while the other side may remain physically unaffected. This is in contrast to a traumatic brain injury where both sides of the body may be affected equally or one more than the other.

The goal of rehabilitation after stroke is to teach you to become as independent as possible. The keystone to stroke rehabilitation is reteaching the brain to do the functions that have been affected by the stroke. The brain has an incredible ability to retrain a different area of the brain to take over the functions of the brain that have been lost due to the stroke. This is called neuroplasticity. “Neuro” refers to the brain cells and “plasticity” refers to the pliable nature of different brain cells to take over lost functions. With rehabilitation, brain cells regenerate, re-establish, and rearrange the needed brain circuits to resume lost functions despite the original cells and pathways having been damaged by the stroke. The brain effectively compensates for the dead or damaged brain cells. In instances where it cannot establish these new connections, rehabilitation works to teach the brain and body to compensate for the disabilities that occur due to the stroke.
Starting rehabilitation as early as possible is important to receive the most benefit. Once you are medically stable in the hospital, rehabilitation may begin as early as 48 hours after a stroke. Once you are discharged from the hospital then regular rehabilitation should continue either at home or at a clinic that specializes in stroke rehabilitation. Because repetition and intense practice is important in neuroplasticity, frequently repeated *physiotherapy* sessions that focus on specific skills that are tailored to each patient’s individual deficits, as well as repeated practice of learned skills is very important. 45 minutes of therapy at least 2-5 times a week, depending on the patient’s goals and individual circumstances, is recommended and shown to be required to make measurable gains in rehabilitation. Although rehabilitation can be effective even years after a stroke, the most notable gains in rehabilitation are made early on in the rehabilitation process so *physiotherapy* should start as soon as possible and be a regular part of the stroke recovery process.
As mentioned, each stroke presentation is unique. Your *physiotherapist* will do an initial assessment of your individual problems and determine what needs to be addressed in your situation and what requires the most attention. They will inquire about your goals regarding returning to your activities of daily living. Working through the physical loss of strength and sensation on one side of your body may also be complicated by other stroke-induced impairments such as visual losses, as well as the ability to understand instructions and the ability to express one’s self (receptive and/or expressive aphasia) or actual difficulty speaking (dysphasia). Apraxia may also be present; this refers to losing the ability to carry out a learned purposeful movement or being unable to plan the steps involved in completing a complex task and doing them in the proper sequence, such as getting out of bed or making a cup of coffee.
Working in conjunction with other rehabilitation professionals such as speech pathologists and occupational therapists will be important in addressing all impairments simultaneously.
Proprioception and Balance
Simply put, proprioception, or kinesthesia, is the ability to know where your joint or limb is in space without looking at it. Proprioception is how we sense the position and movement of our body including our ability to balance.
A large part of stroke rehabilitation will be focused on proprioception and balance. Because one side of the body is affected during a stroke, proprioception and balance are usually severely compromised. Depending on where the stroke occurs in the brain (some areas are more involved in balance) and also depending on the severity of the stroke some patients will have trouble even sitting without losing their balance after a stroke. Others will be ok when sitting but are unable to stand or walk without losing their balance. Your *physiotherapist* will work closely with you to gain the ability to sit, stand and walk, depending on your level of impairment.
Transfers
Transferring from one surface to another can be very difficult after a stroke when one side of your body is not functioning as it used to. Because getting in and out of bed, on and off a chair, on and off the toilet, in and out of the shower/bath and in and out of a car are all important tasks for daily living, your *physiotherapist* will focus on gaining the needed strength and balance to master these tasks as soon as possible.
Strength and Range of Motion
After a stroke one side of the body is affected in its ability to voluntarily move, while the other side of the body may be completely normal. Depending on the severity and location of the stroke the muscles on the affected side may be completely paralysed (flaccid) or they may continue to have some movement available. The upper extremity (shoulder, arm and hand) is generally more adversely affected than the lower extremity (hip, leg and foot). It should be noted that even though initially the upper or lower limb on the affected side may be flaccid, often some movement will return over time with rehabilitation due to neuroplasticity. Some muscles, however, may be permanently paralysed or may not gain enough movement to be used for any purposeful function. Early rehabilitation is important to encourage activation of the muscles and promote neuroplasticity. Your *physiotherapist* will assess the movement of your affected side and work to gain as much motion and strength as possible in any active muscles.
The goal of strengthening is to work towards enough strength and control in order for you to use your affected side as much as you can for activities of daily living, even if it is not as functional as it was prior to your stroke.
Gait
Returning to walking is the ultimate goal for most clients who have had a stroke. Fortunately, many can and will achieve this goal. In order to regain the ability to walk, the lower limb on your affected side will require enough strength, range of motion and control (proprioception) to support your body. In addition, you will require adequate standing and moving (dynamic) balance to achieve the skill of walking. Many patients who have had strokes but are able to walk will require a cane or walker which assists with their balance when on their feet. Your *physiotherapist* will assess your skills and determine if and when working on the skill of walking is appropriate. Your therapist may use a form of biofeedback that helps you see or hear stimuli (rhythmic auditory stimuli) in conjunction with your movement in order to help you improve your walking pattern and cadence.
It is important for individuals to maintain as much independence as possible so your *physiotherapist* will strive towards the goal of ambulation (walking) whenever possible. In cases where ambulation is not feasible then your *physiotherapist* will assist in teaching you how to mobilize in a wheelchair on your own.
Other modalities
Stroke rehabilitation research is ongoing worldwide and new types of treatments are continually being tested for their efficacy. We know for sure that in order to encourage neuroplasticity, regular and ongoing rehabilitation which repeats meaningful tasks and addresses the specific deficits of each patient, including working towards doing functional activities (doing activities that one would do in daily life) is effective. Essentially rehabilitation in this regard is in line with how we would learn any new skill, such as a tennis serve or writing a new language; we would practice repeatedly and regularly the actual skills that are involved in the new task until we can put the skills together into the desired task. There are many types of modalities or treatments that may be trialled within your *physiotherapy* sessions to assist in maximizing the skills gained. For example:
Mirrors: mirrors can be useful to help clients visualize their deficits and assist with proprioception, balance and ambulation. In a special type of mirror therapy your *physiotherapist* may place the mirror between your limbs and cover up your affected limb so that when you move your strong side, it appears to your brain that your weaker side is moving. This may be an effective way to ‘trick’ the brain into thinking that it is moving the weaker side. This can assist in encouraging the weaker side to move on its own.
Constraint Therapy: during this type of therapy the strong side is actually immobilized so that the affected side is forced to do the work.
Bracing: some forms of standard or customized bracing may be used to assist the upper limb and hand as well as the weakness in the foot.
Treadmill Walking: at certain stages of rehabilitation a treadmill can be very effective in retraining ambulation. Depending on your level of function your therapist may choose to use the treadmill with or without a brace which helps to hold you up and support your body weight. Robotic-type electromechanical devices may be used if available to encourage the walking motion.
Visualization: encouraging a mental image of the task at hand is a very effective way to re-teach the affected limb. Your therapist may encourage you to shut your eyes and visualize several times your affected limb doing the task well, and then once you can do this, they will ask you to try doing the task with your affected side.
Virtual reality training: although not widely available, some clinics or therapists may have access to virtual reality technologies which may be useful in rehabilitation.
Aerobic training: for patients who maintain a high level of their functional abilities aerobic training can be incorporated in terms of treadmill training, cycling, or aquatic therapy.
Cycling: for patients who maintain a high level of their functional abilities, cycling may be used as a form of coordination and aerobic training.
Aquatic therapy: for patients who maintain a high level of their functional abilities aquatic therapy can be used for coordination, strength, gait and aerobic training.
Tai Chi: for patients who maintain a high level of their functional abilities tai chi is an effective form of training for balance and proprioception
Force platform training: if available, the feedback from a force plate which measures weight bearing can be used to assist balance and proprioception training
Interdisciplinary Team Review
A stroke affects the whole person; depending on the severity it can physically affect both your upper and lower limbs, your cognition, your vision, your speech and your emotional and mental health. As such, it is important to work with a full multidisciplinary team in order to best treat and manage all affected aspects. Your team may include your doctor, your *physiotherapist*, a speech pathologist, an occupational therapist, a dietician, a psychologist, a social worker, and other health care professionals. Together this team of professionals can address your deficits as a whole and work together to provide you with the most effective treatment to maximize your overall abilities.
Conclusion
 A stroke is a serious medical emergency that requires immediate action in order to achieve the best eventual outcomes. Early medical intervention, as well as early, consistent and ongoing rehabilitation will positively affect your long term capabilities. Physical therapy services at Ari Levine PT, PC can assist you to recover from your stroke and regain your maximum potential.
A stroke is a serious medical emergency that requires immediate action in order to achieve the best eventual outcomes. Early medical intervention, as well as early, consistent and ongoing rehabilitation will positively affect your long term capabilities. Physical therapy services at Ari Levine PT, PC can assist you to recover from your stroke and regain your maximum potential.
Portions of this document copyright MMG, LLC.












 Other tests
Other tests
 A stroke is a serious medical emergency that requires immediate action in order to achieve the best eventual outcomes. Early medical intervention, as well as early, consistent and ongoing rehabilitation will positively affect your long term capabilities. Physical therapy services at Ari Levine PT, PC can assist you to recover from your stroke and regain your maximum potential.
A stroke is a serious medical emergency that requires immediate action in order to achieve the best eventual outcomes. Early medical intervention, as well as early, consistent and ongoing rehabilitation will positively affect your long term capabilities. Physical therapy services at Ari Levine PT, PC can assist you to recover from your stroke and regain your maximum potential.